Operative Vaginal Delivery
BS. Nguyễn Hồng Anh
Operative vaginal delivery (OVD) is birth accomplished with assistance rom orceps or a vacuum-cup device. Once these are applied to the etal head, outward traction generates orces that augment maternal pushing to deliver the etus.
INCIDENCE AND INDICATIONS
From national data, orceps or vacuum-assisted vaginal delivery aided 3.1 percent o births in the United States in 2015. Tis is a decline rom 9 percent in 1990 (Martin, 2017). For these procedures, a vacuum is disproportionately selected, and the vacuum-to-orceps delivery ratio approximates 4:1 (Yeomans, 2010). Most o these procedures are successul in eecting vaginal birth. From 2006 United States data, only 0.4 percent o orceps trials and 0.8 percent o vacuum extraction attempts ailed to result in vaginal birth (Osterman, 2009). In the specic group o nulliparas with term gestations, higher ailure rates o 4.4 and 6.4 percent, respectively, were ound in a study o 25 academic hospitals (Bailit, 2016). I technically sae, termination o second-stage labor by OVD is considered or any condition that threatens the mother or etus and that is likely to be relieved by delivery. O maternal indications, the most common are maternal exhaustion and prolonged second-stage labor. However, a specic, maximum second-stage length beyond which all women should be considered or OVD has not been dened (American College o Obstetricians and Gynecologists, 2019). Other maternal reasons are preexisting or intrapartum conditions that limit eective pushing or warrant expedited delivery. Severe or acute pulmonary compromise, decompensation rom intrapartum inection, neurological disease, and serious cardiac disorders are examples. Frequent etal indications include nonreassuring etal heart rate and premature placental separation (Schuit, 2012).
CLASSIFICATION AND PREREQUISITES
Classication o OVD is summarized in Table 29-1. It emphasizes that station and rotation are the two most important discriminators o risk or both mother and neonate. Station is measured by the number o centimeters, either above or below, an anatomical zero station, which is a line drawn between the ischial spines. Stations range rom –5 to 0 to +5. Procedures are categorized as outlet, low, and midpelvic, and most are low or outlet deliveries. High orceps, in which instruments are applied above 0 station, have no place in current obstetrics. o aid patient selection, the Society or Maternal–Fetal Medicine (2020) published a preprocedural checklist and documentation template. Once station and rotation are determined, the prerequisites listed in able 29-1 are assessed. For vacuum extraction, etuses ideally are not younger than 34 weeks’ gestation because o cranial hemorrhage vulnerability at earlier ages (Åberg, 2014). Also prior to vacuum use, although inrequently used in the United States, etal scalp blood sampling should not have been recently perormed. O requisites, ascertaining correct head position is essential, and Figure 29-1 shows etal skull anatomy. In unclear cases, sonography can help identiy etal orbits and nasal bridge to aid orientation (Ghi, 2018). Regional analgesia is preerable or low or midpelvic procedures. Pudendal blockade may prove adequate or outlet deliveries. As a causative actor, newer epidural methods or placement during early labor do not raise OVD rates (AnimSomuahm, 2018; Liu, 2004).
Te bladder is emptied to provide additional pelvic space and minimize bladder trauma. Urinary retention and bladder dysunction are requent short-term eects o OVD (Mulder, 2012; Piarotti, 2014). Notably, episiotomy and epidural analgesia, both common associates o OVD, also are risks or urinary retention. Retention usually resolves ater 24 to 48 hours o passive catheter bladder drainage (Chap. 36, p. 643).
FIGURE 29-1 Fetal head (A–B) at term showing fontanels, sutures, and various dimensions.MORBIDITY
■ Maternal Morbidity
OVD carries increased risk o certain morbidities or both mother and etus. In general, a higher station and greater degrees o rotation raise procedure diculty and the chance o injury. Morbidity is most properly compared with morbidity rom cesarean delivery and not with that rom spontaneous birth. Tis is the most appropriate comparator because the alternative to indicated OVD is cesarean delivery.
Lacerations
Te very indications that prompt OVD are among those that also increase the need or episiotomy and the likelihood o lacerations (de Leeuw, 2008). Tat said, higher rates o third- and ourth-degree perineal lacerations, vaginal wall lacerations, and less oten cervical tears do complicate OVD compared with spontaneous birth (Friedman, 2015; Gurol-Urganci, 2013; Landy, 2011). Tese rates with OVD are also substantially higher than with cesarean delivery. Tird- and ourth-degree perineal lacerations are grouped as obstetrical anal sphincter injuries (OASIS). In general, these tears more requently attend orceps delivery compared with vacuum extraction, and especially i an episiotomy is midline (Kudish, 2006; O’Mahony, 2010). With OVD, indicated episiotomy rather than routine use is recommended. I required, a mediolateral episiotomy aords greater protection against OASIS than midline incision (GurolUrganci, 2013; Jangö, 2014; van Bavel, 2018). But, shortterm rates o pain and dyspareunia are similar or increased with mediolateral episiotomy (Chap. 27, p. 510). As another OASIS protection, early orceps disarticulation and removal can avoid the ull perineal distention created by the blades and crowning head. Moreover, cessation o maternal pushing during disarticulation or as the head begins to crown allows the clinician sole control o outward orces against the perineum.
Similarly, adding a dedicated assistant to bolster the perineum can lower OASIS rates, and this is our practice (Wan, 2020). Last, OASIS are more common with an occiput posterior (OP) position (Damron, 2004). Tus, manual or orceps rotation to an occiput anterior (OA) position may lower rates o lower reproductive tract injury (Bradley, 2013).
Infection and Subsequent-pregnancy Morbidity
As detailed in Chapter 30 (p. 548), cesarean delivery carries greater maternal morbidity compared with spontaneous birth. For OVD, in one study o more than 1 million births, cesarean delivery, but not OVD, was a risk or peripartum hysterectomy (Spiliopoulos, 2011). Further, avoiding cesarean delivery can minimize rates o subsequent pregnancy complications, such as placenta previa, placenta accreta spectrum, uterine rupture, and adhesion-related surgical organ injury.
In addition, postpartum wound or uterine inection is more requent in women ollowing cesarean compared with OVD (Bailit, 2016; Halscott, 2015). Still, to address peripartum inection, investigators in the ANODE trial randomly assigned nearly 3500 gravidas undergoing OVD to receive either placebo or a single intravenous dose o amoxicillin plus clavulanic acid (Knight, 2019). Te puerperal inection rate was 11 percent ater antibiotic prophylaxis compared with 19 percent in those given placebo. Notably, these inections oten coincide with long labors and multiple cervical examinations, both o which are common with women requiring OVD. Tus, we believe that provision o antibiotics to those undergoing OVD without other inection-related risks warrants urther study. Indeed, the American College o Obstetricians and Gynecologists (2020a) notes that this prophylaxis is reasonable but recommends against routine antibiotic prophylaxis or all women undergoing OVD. However, the College (2020b) does note that a single antibiotic dose with third- and ourth-degree perineal laceration is reasonable. Several studies support this practice (Duggal, 2008; Lewicky-Gaupp, 2015; Stock, 2013a).
Pelvic Floor Disorders
Tis term encompasses urinary incontinence, anal incontinence, and pelvic organ prolapse (POP). OVD has been implicated as a possible risk or each. Proposed mechanisms include structural compromise or pelvic foor denervation secondary to orces exerted during delivery. For urinary incontinence, parity and specically vaginal delivery are risk actors (Gyhagen, 2013; Rortveit, 2003). But, many studies do not support a higher risk rom OVD compared with the risk rom vaginal birth alone (Gartland, 2016; Leijonhuvud, 2011; MacArthur, 2016). Evidence linking anal incontinence with OVD is conficting. Some studies show that OASIS, but not delivery mode, is the main etiological link (Bols, 2010; Evers, 2012; Nygaard, 1997). In contrast, others directly associate OVD with anal incontinence (Dolan, 2010; MacArthur, 2013). But, these studies may not be incongruous—recall that OVD is associated with increased rates o OASIS. Importantly, several studies and reviews have not ound cesarean delivery to be protective long term against anal incontinence (Nelson, 2010). Similarly or POP, evidence linking it to OVD is mixed (Gyhagen, 2013; Volløyhaug, 2015). First, pelvic foor mechanisms leading to POP are complex and incompletely dened (Gordon, 2019). Despite this, obstetrical avulsion o the levator ani muscle rom the pelvic sidewall has been implicated, and OVD, especially orceps delivery, is one risk or this injury (DeLancey, 2007; Dietz, 2008; Friedman, 2019). Again, the pelvic foor injury rather OVD itsel may be the causative agent, as those with OVD but no avulsion did not suer greater POP rates in one recent analysis (Handa, 2019).
■ Perinatal Morbidity
Acute Perinatal Injury
OVD carries higher risk or etal injury than cesarean delivery or spontaneous birth. Both OVD methods are implicated, and actors can include delivery duration and the number o pulls or cup pop-os (Åberg, 2019; Levin, 2019; Miller, 2020). Injuries are more requent with vacuum extraction, and injuries with this device include cephalohematoma, subgaleal hemorrhage, retinal hemorrhage, neonatal jaundice secondary to these hemorrhages, clavicular racture, and scalp lacerations. Cephalohematoma and subgaleal hemorrhage are both extracranial lesions illustrated in Figure 33-2 (p. 608). Shoulder dystocia has been linked to both methods (Dall’Asta, 2016). Forceps delivery has higher rates o acial nerve injury, brachial plexus injury, depressed skull racture, and corneal abrasion (American College o Obstetricians and Gynecologists, 2020a; Demissie, 2004; Dupuis, 2005). With intracranial hemorrhage, some studies have associated vacuum extraction with higher rates, whereas others show similar rates with either OVD method (owner, 1999; Wen, 2001; Werner, 2011).
Compared with cesarean delivery, OVD carries higher risk o extracranial hematomas, ractures, nerve injuries, retinal hemorrhage, and head lacerations. However, rates o etal acidemia or hypoxic encephalopathy are not higher with OVD compared with second-stage cesarean delivery (Bailit, 2016; Contag, 2010; Walsh, 2013). Intracranial hemorrhage rates are similar among newborns delivered by vacuum extraction, orceps, or cesarean delivery during labor (owner, 1999). But, intracranial hemorrhage rates are higher than among those delivered spontaneously or by cesarean delivery beore labor. Tese authors suggest that the common risk actor or intracranial hemorrhage is abnormal labor. Werner and associates (2011), in their evaluation o more than 150,000 singleton deliveries, reported that orceps delivery was associated with ewer total neurological complications that included seizures, intraventricular hemorrhage, and subdural hemorrhage compared with vacuum-assisted birth or any cesarean delivery. Compared with rotational OVD, second-stage cesarean delivery has similar maternal and neonatal morbidity rates (Aiken, 2015; Bahl, 2013; Stock, 2013b). For example, in their large series, empest and associates (2013) ound similar morbidity rates among malpositioned etuses during second-stage labor that underwent Kielland rotation, rotational vacuum extraction, or emergency cesarean delivery.
Midorceps by denition are perormed rom a higher station. Te bulk o data are rom older studies, and most show comparable neonatal morbidity between low and midorceps procedures (Dierker, 1985; Gilstrap, 1984). In a recent report also comparing these two, Ducarme and coworkers (2015) ound comparable neonatal and maternal composite morbidity scores. Comparing midpelvic OVD and second-stage cesarean delivery, most studies support neonatal saety (Bashore, 1990; Cibils, 1990; Hagadorn-Freathy, 1991). But, others have ound increased rates o trauma and umbilical cord blood acidemia with midorceps delivery (Robertson, 1990). More recently, Muraca and associates (2018) compared midpelvic OVD methods against second-stage cesarean delivery. For the indication o dystocia, etal and maternal morbidity composite scores were higher with OVD. With distress as the indication, the neonatal morbidity score was greater only with midpelvic vacuum-assisted OVD, whereas the maternal morbidity score was higher only with midorceps. In another study comparing both midpelvic OVD methods, maternal morbidity was greater with orceps, and neonatal morbidity diered only in a higher cephalohematoma rate with vacuum-assisted delivery (Baerthlein, 1986).
Mechanisms of Acute Injury
Te types o etal injury with OVD can usually be explained by the orces exerted. In cases o cephalohematoma or subgaleal hemorrhage, suction and perhaps rotation during vacuum extraction may lead to a primary vessel shearing. Intracranial hemorrhage may result rom skull racture that lacerates vessels or rom vessel rupture alone due to exerted orces. With acial nerve palsy, one o the orceps blades compresses the nerve against the acial bones. o explain brachial plexus injury, owner and Ciotti (2007) proposed that as the etal head descends down the birth canal, the shoulders may stay above the pelvic inlet. Tus, similar to shoulder dystocia at the symphysis, this “shoulder dystocia at the pelvic inlet” is overcome by traction orces but with concomitant stretch on the brachial plexus.
Long-term Infant Morbidity
Evidence regarding long-term neurodevelopmental outcomes in children born by OVD is reassuring (Seidman, 1991; Wesley, 1992). Moreover, no association between orceps delivery and later epilepsy was ound in a cohort study o more than 21,000 births (Murphy, 2004). In their review, O’Callaghan and colleagues (2011) reported no link between cerebral palsy and OVD. Last, the incidence o neurodevelopmental morbidity was similar in those undergoing successul orceps delivery, ailed orceps with cesarean delivery, or cesarean delivery without orceps in one study (Bahl, 2007). Similarly, with midpelvic OVD, long-term neurodevelopment is not harmed in most analyses (Dierker, 1986; Friedman, 1984; Nilsen, 1984; Wesley, 1993).
Trial of Operative Vaginal Delivery
I an attempt to perorm OVD is expected to be dicult, it should be considered a trial. Moving the woman to an operating room or this attempt, which could be ollowed by immediate cesarean delivery i OVD ails, has merit. I orceps cannot be satisactorily applied, the procedure is stopped. Either a trial o vacuum-assisted delivery or cesarean delivery is then per- ormed. With the ormer, i the etus does not descend with traction, the trial should be abandoned and cesarean delivery perormed.
With such caveats, cesarean delivery ater an OVD attempt was not associated with adverse neonatal outcomes i the etal heart rate was concurrently reassuring (Alexander, 2009). A similar study evaluated 122 women who had a trial o midpelvic OVD in a setting with ull preparations or cesarean delivery (Lowe, 1987). Investigators ound no signicant dierence in immediate neonatal or maternal morbidity compared with that o 42 women delivered or similar indications by cesarean but without such a trial. Conversely, in 61 women who had “unexpected” vacuum or orceps ailure in which there was no prior preparation or immediate cesarean delivery, neonatal morbidity was higher.
Some actors associated with OVD ailure are persistent OP positions and birthweight >4000 g (Ben-Haroush, 2007; Verhoeven, 2016). However, Palatnik and coworkers (2016) ound that risk actors poorly predicted success. In general, to avert morbidity with ailed OVD, the American College o Obstetricians and Gynecologists (2020a) cautions that these trials should be attempted only i the clinical assessment suggests a successul outcome. We also emphasize proper training
Sequential instrumentation most oten involves an attempt at vacuumassisted OVD ollowed by one with orceps. Tis sequence likely refects the overall higher completion rate with orceps. However, this practice signi- cantly raises etal trauma risks (Dupuis, 2005; Gardella, 2001; Murphy, 2011). Te American College o Obstetricians and Gynecologists (2020a) recommends against the sequential use o instruments unless there is a “compelling and justiable reason.”
FORCEPS DELIVERY
■ Design
Forceps reers to the paired instrument, and each member o this pair is called a branch. Branches are designated let or right according to the side o the maternal pelvis to which they are applied (Fig. 29-2A). Each branch has our components: blade, shank, lock, and handle (see Fig. 29-2B). Each blade has a toe, a heel, and two curves. O these, the outward cephalic curve conorms to the round etal head, whereas the upward pelvic curve corresponds to the curve o the birth canal. Some blades are solid, meaning smooth on both suraces. Others have an opening within or a depression along the blade surace and are termed enestrated or pseudoenestrated, respectively. A true window in the blade reduces the degree o head slippage within the blades during orceps rotation. Disadvantageously, it can increase blade thickness and riction against the vaginal wall. With pseudoenestration, the orceps blade is smooth on the outer maternal side but indented on the inner etal surace. Te goal is to reduce head slipping yet improve the ease and saety o application and removal o orceps. In most situations, however, despite these subtle dierences, any are appropriate.
Te blades are connected to shanks, which may be parallel or overlapping. Parallel shanks limit compression o blades against the etal head and may be helpul with deliveries employing greater orces. Tese shanks, however, add width against the introitus. In comparison, overlapping shanks raise compression orces but distend the perineum less. Tis may oer greatest advantage or outlet deliveries.
Locks are ound on all orceps and help to connect the right and let branches and stabilize the instrument. Tey can be located at the end o the shank nearest to the handles (English lock), at the ends o the handles (pivot lock), or along the shank (sliding lock). Although varied in design, handles, when squeezed, raise compression orces against the etal head. Tus, orces to consider include traction and compression.
FIGURE 29-2 A. Simpson forceps have fenestrated blades, parallel shanks, and English lock.The cephalic curve accommodates the fetal head. B. Luikart forceps have pseudofenestrated
blades, overlapping shanks, a sliding lock, and tongue-in-groove handles. The pelvic curve
(black curve) is marked in this example.
■ Blade Application and Delivery
Forceps blades grasp the head and are applied according to etal head position. I the head is in an OA position, two or more ngers o the right hand are introduced inside the let posterior portion o the vulva and advanced into the vagina beside the etal head. Te handle o the let branch is grasped between the thumb and two ngers o the let hand (Fig. 29-3). Te blade tip is then gently introduced along the posterior let vaginal wall. It is swept upward and inward between the etal head and the palmar sur- ace o the ngers (Fig. 29-4). Tis blade can be held in position by an assistant. For application o the right blade, two or more ngers o the let hand are introduced into the right posterior portion o the vagina to serve as a guide or the right blade. Tis blade is held in the right hand and introduced into the vagina. With each blade, the thumb is positioned behind the heel, and most o the insertion orce comes rom this thumb (Fig. 29-5). I the head is positioned in a let OA (LOA) or right OA (ROA) position, then the lower o the two blades is typically placed rst.
FIGURE 29-3 For OA or LOA positions, the left handle of the forceps is held in the left hand. The blade is introduced into the left side of the pelvis between the fetal head and the fingers of theoperator’s right hand
FIGURE 29-4 Insertion arc of the blade. Importantly, the thumb of the right hand, not shown here, guides the blade during placement
FIGURE 29-5 In applying the second blade, insertional force is generated mainly by the thumb. (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)
FIGURE 29-6 A. The forceps are symmetrically placed and articulated. B. The vertex is OA. (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)
FIGURE 29-7 If LOA, the vertex is rotated from this position to OA (arrow). (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)
FIGURE 29-8 With low forceps, the direction of gentle traction for delivery of the head is indicated (arrows). (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)
FIGURE 29-9 Branches are removed in the opposite order from that in which they were originally placed. The fingers of the right hand, covered by a sterile towel, bolster the perineum. The thumb is placed directly on the head to prevent sudden egress. (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)
Te blades are constructed so that their cephalic curve is closely adapted to the sides o the etal head (Fig. 29-6). Te etal head is perectly grasped only when the long axis o the blades corresponds to the occipitomental diameter (see Fig. 29-1). As a result, most o the blade lies over the lateral ace Suboptimal blade placement can increase morbidity (Ramphul, 2015). For OA positions, appropriately applied blades are equidistant rom the sagittal suture, and each blade is equidistant rom its adjacent lambdoid suture. In OP positions, blades are symmetrically placed relative to the sagittal suture and to each coronal suture. Ater correct positioning, the branches can be articulated. I branches do not articulate, the blade’s relationships to the sutures are reassessed. Applied in this way, orceps should not slip, and traction may be applied most advantageously. With most orceps, i one blade is applied over the brow and the other over the occiput, the instrument cannot be locked, or i locked, the blades will slip o when traction is applied.
With both branches in place, slow articulation o the handles will also typically correct mild asynclitism. For greater asynclitism, Luikart orceps can be placed and once positioned, one handle will extend urther than the other along their long axis. Asynclitism is resolved by pulling and/or pushing each respective branch within the sliding lock along the instrument’s long axis until the nger guards align. Once blades are placed satisactorily, rotation to OA position is perormed beore traction is applied (Fig. 29-7). Next, gentle, intermittent, downward and outward traction is exerted concurrent with maternal eorts until the perineum begins to bulge. For most stations, the initial direction o traction is downward and brings the head beneath the symphysis.
With head descent, the vector o orces changes continuously and are gradually directed upward (Fig. 29-8). During the birth o the head, mechanisms o spontaneous delivery should be simulated as closely as possible. As a teaching tool or this, a Bill axis traction device can be attached over the nger guards o most orceps. Te instrument has an arrow and indicator line. When the arrow points directly to the line, traction is along the path o least resistance.
It is impossible to ascertain the amount o orce exerted by orceps or an individual patient. Tus, traction is ideally intermittent and relieved between contractions, as in spontaneous labor. Except when urgently indicated, delivery should be su- ciently slow, deliberate, and gentle to prevent undue head compression. It is preerable to apply traction only with each uterine contraction. Maternal pushing will augment these eorts. With traction, as the occiput distends the vulva, an episiotomy may be perormed i needed. Te delivery may be completed in several ways. Some clinicians keep the orceps in place to control the head. However, this blade volume adds to vulvar distention and raises risks or laceration or episiotomy. o prevent this, the orceps may be removed, and delivery is then completed by maternal pushing (Fig. 29-9). Importantly, i blades are disarticulated and removed too early, the head may recede and prolong delivery. Pushing in some cases may be aided by the modied Ritgen maneuver. We emphasize bolstering o the perineum to control outward orces.
■ Manual Rotation
In many cases, O and OP head positions are oten imper- ectly fexed and present a wider head diameter. Tis can slow etal descent and lengthen second-stage labor. By manually rotating the etal occiput into the anterior pelvis (OA positions), cephalopelvic proportions improve to help hasten spontaneous birth. Tis is usually reserved or second-stage labor. Compared with no attempt, manual rotation is associated with lower rates o cesarean delivery, OVD, severe perineal laceration, and chorioamnionitis (Blanc, 2021; Shaer, 2011). I OVD is still required, the new OA position lowers rates o perineal trauma.
In the simplest cases, digital rotation can correct O or OP positioning. With head molding, the sutures override one another to create a bony ridge. wo ngers hooked against this ridge and orces directed parallel to the skull can rotate the occiput toward the anterior pelvis. Tis is done between contractions, and advancements are then held in place during pushing. Progressive degrees o rotation are attained with each attempt, and several may be needed to ultimately rotate the occiput into the anterior pelvis.
Instead, with manual rotation, an open hand is inserted into the vagina. For ROP position, the right palm cups the etal head and straddles the sagittal suture. Te operator’s ngers wrap to one side o the etal ace, and the thumb extends along the other side. Rotation is clockwise to bring the occiput to an ROA position (Fig. 29-10). With LOP position, rotation is counterclockwise with the let palm. Tree actions are perormed simultaneously between contractions. Te etal head is fexed to provide a smaller diameter or rotation and subsequent descent within the pelvis. Next, slight destationing o the etal head moves the head to a level in the maternal pelvis with sucient room to complete the rotation. Importantly, destationing should not be conused with disengaging the etal head, which is proscribed. Tird, we and others preer also to place the other hand externally on the corresponding side o the maternal abdomen to pull the back o the etus up and toward the midline in synchrony with internal head rotation. Barth (2015) provides an excellent summary o this technique.
Le Ray and associates (2007, 2013) reported a success rate >90 percent with manual rotation. Complication were uncommon. In their report o 796 rotations, no cords prolapsed. wo women sustained cervical lacerations, which required simple vaginal repair. Notably, this study allowed rotations at advanced cervical dilation prior to second-stage labor, which may have enhanced cervical injury risk. In 71 percent, etal heart rate (FHR) was normal during rotation, but severe FHR abnormalities were noted in 10 percent. However, the need or cesarean delivery ater successul manual rotation was not associated with FHR abnormalities. Failure to rotate the head does not mandate cesarean delivery, and options are described next.
FIGURE 29-10 A. Manual rotation using the left hand, palm-up, to rotate from ROP. B. The head is flexed and destationed during clockwise rotation to reach an OA position. (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)■ Persistent Occiput Posterior Positions
In cases with persistent OP positioning, the head may spontaneously deliver OP, may be manually or instrumentally rotated to an OA position, or may be delivered OP by orceps or vacuum (Bertholdt, 2019). In many cases, the cause o a persistent OP position and o the diculty in accomplishing rotation is an anthropoid pelvis. Tis architecture opposes rotation and predisposes to posterior delivery (Fig. 2-16, p. 29).
FIGURE 29-11 Outlet forceps delivery from an OP position. The head should be flexed after the bregma passes under the symphysis.FIGURE 29-12 Kielland forceps. The characteristic features are minimal pelvic curvature (A), sliding lock (B), and light weight.
With orceps delivery rom an OP position, downward and outward traction is applied until the base o the nose passes under the symphysis (Fig. 29-11). Te handles are then slowly elevated until the occiput gradually emerges over the perineum’s ourchette. Te orceps are directed downward again, and the nose, mouth, and chin successively emerge rom the vulva.
OP delivery causes greater vulvar distention, and an episiotomy may be needed. OP deliveries have a higher incidence o severe perineal lacerations and o extensive episiotomy compared with OA positions (de Leeuw, 2008; Pearl, 1993). Also, newborns undergoing OVD rom OP positions have a higher incidence o Erb and acial nerve palsies, 1 and 2 percent, respectively, than those delivered rom OA positions. As expected, rotations to OA ultimately decrease perineal delivery trauma (Bradley, 2013).
For orceps rotations rom an OP to OA position, Kielland orceps are preerred because they have a less pronounced pelvic curve (Fig. 29-12). Cunningham and Gilstrap’s Operative Obstetrics, 3rd edition oers a more detailed description and illustration o this Kielland orceps procedure (Yeomans, 2017).
■ Occiput Transverse Positions
With occiput transverse (O) etal head positions, rotation is required or delivery. For this, the head may be manually or instrumentally rotated into an OA position. Manual rotation was described earlier in that section (p. 540). Forceps rotation by experienced operators can oer high success rates with minimal maternal morbidity (Burke, 2012; Stock, 2013b). Either standard orceps or specialized orceps, such as Kielland orceps, are used. With the latter, each handle has a small knob, and branches are placed so that this knob aces the occiput.
FIGURE 29-13 A. Application of the right branch of the Kielland forceps to a head in LOT position. The knob on this branch (colored blue) will ultimately face the occiput. B. The right branch is wandered to its final position behind the symphysis. C. Insertion of the left branch of the Kielland forceps directly posterior along the hollow of the sacrum. This branch is inserted to the maternal right of the anterior branch to aid in engaging the sliding lock. (Reproduced with permission from Yeomans ER: Operative vaginal delivery. In Yeomans ER, Hoffman BL, Gilstrap LC III, et al (eds): Cunningham and Gilstrap’s Operative Obstetrics, 3rd ed. New York, NY: McGraw Hill; 2017.)Kielland described two methods o applying the anterior blade. In this example, placement with a let O (LO) position is described. With the wandering method, the anterior blade is rst introduced into the posterior pelvis (Fig. 29-13). Te blade is then arched around the ace to an anterior position. o permit this sweep o the blade, the handle is held close to the let maternal buttock throughout the maneuver. Te second blade is introduced posteriorly, and the branches are locked.
Ater checking the application, the provider pulls the handles o the Kielland orceps slightly to the patient’s right to fex the etal head and create a smaller diameter or rotation. Te rst and second ngers o the let hand are placed over the nger guards with the palm against the handles. Tis palm aces the maternal let. Concurrently, the rst two ngers o the operator’s right hand are placed against the anterior lambdoid suture. Te etal head is then elevated and slightly destationed. For rotation in a counterclockwise direction, the wrist o the let hand supinates, to direct this palm upward. Simultaneously, two ngers o the right hand press against the lambdoid suture ridge. Tis ensures that the etal head turns with the blades and does not slip. As a newer adjunct, abdominal sonography can ollow and document head rotation (Hinkson, 2021).
Te second type o blade application introduces the anterior blade with its cephalic curve directed upward to curve under the symphysis. Ater it has been advanced ar enough toward the upper vagina, it is turned on its long axis through 180 degrees to adapt the cephalic curvature to the head. Te second blade is introduced posteriorly, and the branches are locked. Ater rotation o the etal occiput into the anterior pelvis, two acceptable methods or delivery are available. In one, the operator applies traction on the Kielland orceps using a bimanual grip described previously or conventional orceps (p. 539). When the posterior ontanel has passed under the subpubic arch, the handles can be elevated to the horizontal, but no urther. Raising the handles above the horizontal may cause vaginal sulcus tears because o the reverse pelvic curve (Dennen, 1955). Alternatively, the Kielland orceps can be removed ater rotation and replaced with conventional orceps. With this approach, moderate traction is rst employed to seat the head beore switching instruments.
■ Face Presentations
FIGURE 29-14 Vacuum delivery systems. A. The Kiwi OmniCup contains a handheld vacuum-generating pump, which is attached via flexible tubing to a rigid plastic mushroom cup. B. The MityvacMystic II MitySoft Bell Cup has a soft bell cup attached by a semirigid shaft to a handheld pump
With a mentum anterior ace presentation, OVD is an option.
Te blades are applied to the sides o the head along the occipitomental diameter, with the pelvic curve directed toward the neck (see Fig. 29-1). Downward traction is exerted until the chin appears under the symphysis. Ten, by an upward movement, the ace is slowly extracted, with the nose, eyes, brow, and occiput appearing in succession over the anterior margin o the perineum. Forceps should not be applied to the mentum posterior presentation because vaginal delivery is impossible except in very small etuses.
VACUUM-ASSISTED DELIVERY
■ Vacuum Extractor Design
With vacuum-assisted OVD, suction is created within a cup placed on the etal scalp such that traction on the cup aids etal birth. In the United States, vacuum extractor is the pre- erred term, whereas in Europe it is commonly called a ventouse (Fig. 29-14). Teoretical benets o this tool compared with orceps include simpler requirements or precise positioning on the etal head and avoidance o space-occupying blades within the vagina to help mitigate maternal trauma.
Vacuum devices contain a cup, shat, handle, and vacuum generator. Vacuum cups are metal or plastic and dier in their shape, size, and reusability. In the United States, plastic cups are generally preerred. O these, the sot cup is a pliable bell-shaped dome, whereas the rigid type has a rm fattened mushroom-shaped cup and circular ridge around the cup rim (Table 29-2). When compared, rigid mushroom cups generate signicantly more traction orce (Homeyr, 1990; Muise, 1993). With OP positions or with asynclitism, the fatter cup also permits improved placement at the fexion point, which is typically less accessible with these head positions. Te tradeo is that the fatter cups have higher scalp laceration rates.
Tus, many manuacturers recommend sot bell cups or more straightorward OA deliveries Several investigators have compared outcomes with various rigid and sot cups. Metal cups yield higher success rates but greater rates o scalp injuries, including cephalohematomas (O’Mahony, 2010). In another study, Kuit and colleagues (1993) ound that the only advantage o the sot cups was a lower incidence o scalp injury. In a review, Vacca (2002) concluded that ewer scalp lacerations occurred with the sot cup, but that the rate o cephalohematomas and subgaleal hemorrhage was similar between sot and rigid cups. Importantly, high-pressure vacuum generates large amounts o orce regardless o the cup used (Duchon, 1998). Aside rom the cup, the shat that connects the cup and handle may be fexible or semifexible. ubing-like fexible shats may be preerred or OP positions or asynclitism to permit better seating o the cup. Last, the vacuum generator may be handheld and actuated by the operator, or it may be held and operated by an assistant.
■ Technique
FIGURE 29-15 Drawing demonstrates correct cup placement at the flexion point. Along the sagittal suture, this spot lies 3 cm from the posterior fontanel and 6 cm from the anterior fontanel.An important step in vacuum-assisted OVD is proper cup placement over the fexion point. Tis pivot point maximizes traction, minimizes cup detachment, fexes the neck, and delivers the smallest head diameter through the pelvic outlet. Tis improves success rates, lowers scalp injury rates, and lessens perineal trauma because the smallest head diameter distends the vulva (Baskett, 2008).
Te fexion point is ound along the sagittal suture, approximately 3 cm rom the posterior ontanel’s center and approximately 6 cm rom the anterior ontanel’s center. Because most cup diameters measure 5 to 6 cm, when properly placed, the cup rim lies at the posterior ontanel’s border and 3 cm rom the anterior ontanel (Fig. 29-15). Placement o the cup more anteriorly on the etal cranium—near the anterior ontanel—is ideally avoided as it leads to neck extension during traction unless the etus is small. Such placement delivers a wider head diameter through the vaginal opening. Last, asymmetrical placement relative to the sagittal suture may worsen asynclitism. Cup placement in OA positions is seldom dicult. In contrast, i the indication or delivery is ailure to descend caused by occipital malposition, cup positioning can be dicult.
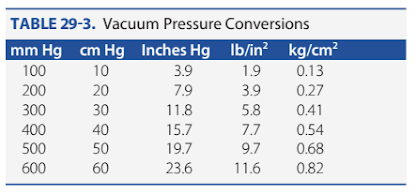
During cup placement, maternal sot tissue entrapment predisposes the mother to lacerations and virtually ensures cup dislodgement, colloquially called a “pop o.” Tus, the entire cup circumerence should be palpated both beore and ater the vacuum has been created and again prior to traction to exclude such entrapment. Gradual vacuum creation is advocated by some and is generated by increasing the suction in increments o 0.2 kg/cm2 every 2 minutes until a total negative pressure o 0.8 kg/cm2 is reached (Table 29-3). Tat said, other studies have shown that negative pressure can be increased to 0.8 kg/cm2 in <2 minutes without a signicant dierence in ecacy or in maternal and etal outcomes (Suwannachat, 2011, 2012).
Once suction is created, the instrument handle is grasped, and traction is initiated. Similar to orceps delivery, traction angles mirror that in Figure 29-8 and should be steady without jerking or rocking. Te number o needed pulls increases with higher station but typically ranges rom one to our. Eorts are intermittent, and each pull is coordinated with maternal pushing. Manual torque to the cup is avoided as it can cause cup displacement or cephalohematomas and, with metal cups, “cookie-cutter”– type scalp lacerations. Tus, OA oblique positions are corrected not by rotation, but solely by downward outward traction. Similarly, or OP positions, rotational orces should not be applied.
Instead, with correct fexion point placement and line o traction, the head will usually rotate by itsel (van den Akker, 2019). During pulls, the operator should place the nondominant hand within the vagina, with the thumb on the extractor cup and one or more ngers on the etal scalp. So positioned, descent o the presenting part can be judged and the traction angle can be adjusted with head descent. In addition, the relationship o the cup edge to the scalp can be assessed to help detect cup separation.
Between contractions, some physicians will lower the suction levels to decrease scalp injury rates, whereas others will maintain suction in cases with a nonreassuring FHR to aid rapid delivery. No dierences in maternal or etal outcome were noted i the vacuum level was decreased between contractions or i an eort was made to prevent etal loss o station (Boll, 1997). Once the head is delivered, the vacuum pressure is relieved and the cup removed.
Vacuum extraction should be considered a trial. Without early and clear evidence o descent toward delivery, an alternative delivery approach should be adopted. As a general guideline, progressive descent should accompany each traction attempt. Neither data nor consensus are available regarding the number o pulls required to eect delivery, the maximum number o cup pop-os that can be tolerated, or optimal total duration o the procedure. Some manuacturers have recommendations regarding these (Clinical Innovations, 2018; CooperSurgical, 2018).
During a vacuum-assisted delivery trial, cup dislodgement due to technical ailure or less than optimal placement should not be equated with dislodgement under ideal conditions o exact cup placement and optimal vacuum maintenance. echnical ailures may merit either additional attempts at cup placement or, alternatively, a trial o orceps (Ezenagu, 1999; Williams, 1991). Te least desirable cases are those in which traction without progress or multiple disengagements occur ollowing correct cup application and appropriate traction. As with orceps, clinicians should embrace a willingness to abandon attempts at vacuum-assisted delivery i satisactory progress is not made (American College o Obstetricians and Gynecologists, 2020a).
TRAINING
As the OVD rate has declined, so have opportunities or resident training (Fitzwater, 2015; Kyser, 2014). In accredited programs, the median number o these procedures completed by trainees has reached critically low levels, and or recent graduates it approximated only 20 (Accreditation Council or Graduate Medical Education, 2019; Dildy, 2016). For residents completing training in 2021, the Accreditation Council or Graduate Medical Education (2020) minimum requirement is 15 procedures. o adapt, residency programs should have readily available skilled operators to teach these procedures by simulation as well as through actual cases (Spong, 2012). In one study, a 59-percent increase in orceps deliveries over 2 years was related to a single experienced and proactive instructor assigned to teach orceps to residents in labor and delivery (Solt, 2011). In another, ollowing implementation o a ormal education program that included a manikin and pelvic model simulation, rates o neonatal morbidity and o severe maternal cervical, labial, and vaginal lacerations declined. However, OASIS rates were unchanged (Cheong, 2004). Gossett and associates (2016) ound a 22-percent reduction in the OASIS rate ollowing an OVD simulation curriculum

















Nhận xét
Đăng nhận xét