Chapter 8.2 Conventional Laparoscopic Hysterectomy Including Laparoscopic Supracervical Hysterectomy. Operative Techniques
Chapter 8.2 Conventional Laparoscopic Hysterectomy Including Laparoscopic
Supracervical Hysterectomy
GENERAL PRINCIPLES
Definition
Hysterectomy is the most common nonobstetric operation performed in the
United States with 602,457 procedures performed in 2003 alone.1 It is also
the most common surgical procedure performed on women in Western
countries, with 23.3% of women aged 18 years or older undergoing the
procedure.2 The primary indication listed for hysterectomy are fibroids
(31%), uterine prolapse (14.5%), endometriosis (11%), abnormal uterine
bleeding (14%), and cancers of the genital tract (10%).3 Cohen revisited this
using the 2009 United States Nationwide Inpatient Sample and found a
decrease in the total number of hysterectomies performed, 479,814, in
women 18 years of age or greater,4 with 86.6% performed for benign
indications. Note that the decrease in numbers does not necessarily reflect a
drop in the actual number of hysterectomies performed as this and the
previous studies looked primarily at inpatient statistics and does not reflect
the shift to the outpatient performance of these procedures. In fact, Loring et
al.,5 looking at a large retrospective review of hysterectomies performed
between 2004 and 2012, noting that, in 2004, 2 of 194 laparoscopic
hysterectomies were performed in an outpatient setting, whereas, by 2012,
85% (293/344) were performed as outpatient procedures. Still, the study is
instructive in that 56% were completed abdominally, 20.4% were performed
laparoscopically, 18.8% done vaginally, and 4.5% performed with robot
assistance. Furthermore, Wright et al.6 documented a change in the
performance of hysterectomy for benign indications with the introduction of
the robot between 2007 and 2010. In his study, there were 40% abdominal,
30.5% laparoscopic, 9.5% robot-assisted, and 19.9% vaginal showing that
robotic and conventional laparoscopic approaches continue to decrease the
numbers of abdominal procedures, although 40% or more are still done as an
open laparotomy.
The access to laparoscopic minimally invasive hysterectomy also appears to
be related to patient socioeconomic status and geographic location. Patel et
al.7 studied a retrospective cohort of 32,436 patients from the 2010
Healthcare Cost and Utilization Project and noted 32% of the patients
underwent laparoscopic hysterectomy (LH) compared to 67% abdominalhysterectomy. Stratifying this, women most likely to undergo LH were less
than 35, Caucasian, and privately insured. Geographically in the United
States, women in the Northeast were far more likely to have an LH compared
to the Midwest and South. Our urban hospitals were more likely than rural,
and teaching hospitals more likely than nonteaching, to offer LH with
government-owned hospitals least likely to offer LH.
The goal of this chapter is to give the reader the tools to advance from the
performance of hysterectomy by laparotomy to a laparoscopic, minimally
invasive approach for most procedures.
Anatomic Considerations
Minimally invasive hysterectomy includes total laparoscopic hysterectomy
(TLH), laparoscopic supracervical hysterectomy (LSH), robotic-assisted
hysterectomy (RAH), and laparoscopic-assisted vaginal hysterectomy (LAVH).
The basic technique for the laparoscopic portion of all of the subgroups is
similar and will be described below as either the TLH or LSH.
There are few contraindications for the TLH approach because this
technique can be used in both benign and malignant conditions. Additionally,
most large uteri can be efficiently addressed using conventional laparoscopic
techniques by an experienced surgical team. Kovac8 outlined three basic
technical issues to determine the route of hysterectomy for benign disease as
they are the difficulties that make most gynecologists apprehensive:
1. Adequacy of the vaginal passageway (e.g., virginity, orthopedic restrictions
to the lithotomy position, and a narrow vagina of <2 fingerbreadths,
especially at the apex of the vagina)
2. The size of the uterus (e.g., leiomyomata)
3. Potential, severe, extrauterine risk factors suggestive of serious pelvic
disease (e.g., endometriosis, adnexal pathology, and adhesions)
Though Kovac originally described an algorithm of obstacles for the
performance of vaginal hysterectomy, the use of conventional laparoscopy
circumvents these obstacles and allows for a minimally invasive solution for
each issue.
Particular consideration must also be paid to obesity in the performance of
laparoscopic surgery. This affects up to 36.5% of Europeans and more than
39.5% of American patients. Guraslan and colleagues9 completed a
retrospective review of 153 patients undergoing TLH stratified by BMI. The
rate of conversion to laparotomy (9.8%), blood loss, total complications
(5.9%), and length of stay did not vary between the groups and they
concluded that LH was safe and feasible in the obese and morbidly obese
population. This was echoed by Mathews10 though they noted potential issues
with increased abdominal pressure and Trendelenburg positioning resulting inincreased airway pressure and end-tidal CO2, in obese versus nonobese
patients. Increased BMI did not appear to be associated with differences in
blood loss, duration of surgery, length of stay, or complication rates.
Additionally, a relative contraindication to laparoscopy was thought to be
the presence of a ventriculoperitoneal shunt. Cobianchi and colleagues11
examined this in a case series and literature review. They concluded that the
current generation valves were unlikely to cause issues with gas leakage
under 80 mm Hg, which is well below that of the current standard insufflation
pressures of 10 to 15 mm Hg. A possible exception is laparoscopy
immediately following a newly implanted shunt for both adults and children.
IMAGING AND OTHER DIAGNOSTICS
Gynecologic diagnostic centers use pelvic ultrasound as the first-line imaging
technique for evaluation of gynecologic complaints such as pelvic pain,
abnormal uterine bleeding, and pelvic masses. This has been the primary
imaging modality of uterine evaluation, showing the number and extent of
fibroids, presence of endometrial disease, and presence and characterization
of adnexal masses. With the controversies surrounding power morcellation
and undetected malignancy, diffusion-weighted MRI and diffusion tensor
imaging have been shown to accurately diagnose preoperatively endometrial,
myometrial, and cervical malignancies with great accuracy,12 though tissue
diagnosis is the gold standard. In the absence of this, traditional MRI is a
reasonable diagnostic tool for use in larger uteri prior to hysterectomy,
particularly in the perimenopausal age range when malignancy is more
common. Blood tumor markers, most notably CA125, have been used but
with limited success. CA125 is elevated with uterine tumors, dependent on
size, adenomyosis, and other inflammatory conditions in the abdomen,
making it of limited diagnostic use. The combination of MRI and serum
fractionated LDH may have a role for planning the surgical approach in
suspicious myometrial lesions.
PREOPERATIVE PLANNING
Proper preoperative assessment will facilitate an efficient procedure. Patients
for which hysterectomy is being considered should have a recent pap smear
and an endometrial biopsy, as clinically indicated, to rule out cancerous or
precancerous processes. Imaging, as suggested above, should be performed to
document uterine and adnexal pathology.
Decisions must be made with the patients regarding hysterectomy type and
approach. The mode of surgical approach is decided between total abdominal
hysterectomy (TAH), transvaginal hysterectomy (TVH), or LH, and the type
of hysterectomy is determined between LSH and TLH. Decisions must bemade as to whether to remove or to keep the cervix in particular. Although
ACOG guidelines continue to recommend vaginal hysterectomy in most cases,
recent studies question that approach. Allam et al.13 completed a randomized
controlled trial which found that although TLH had a longer operating time,
there was less blood loss, fewer complications, and less postoperative pain
than with TAH or VH. Similarly, Pokkinen et al.14 noted reduced need for
analgesics in LH compared with vaginal hysterectomy.
Though supracervical hysterectomy has been performed as long as total
hysterectomy, there are no studies that conclusively define the optimal
procedure. Nesbitt-Hawes15 concluded that, given the currently available
evidence, all forms of hysterectomy should be offered to women requiring
hysterectomy. She noted that it could not be stated that LSH prevents longterm pelvic organ prolapse, offer improved sexual function, or reduce
operative risk, though it does provide faster return to work. In a recent study
from Italy, however, Saccardi et al.16 noted women in their LSH group
reported a greater ease of recovery of sexual function as opposed to TLH.
Complicating the decision-making on the type of hysterectomy is the effect
of TLH and LSH on ovarian reserve. Yuan and colleagues17 looked at ovarian
reserve in patients undergoing total versus supracervical hysterectomy by
assessing anti-müllerian hormone. Their data show serum AMH levels
decreased significantly at 4 months posthysterectomy in patients in their 30s
and 40s, with a much greater decrease in patients having a TLH over those
with LSH. These data suggest that LSH is better than TLH in preserving
ovarian function, and need to be considered when discussing with your
patient.
SURGICAL MANAGEMENT
Positioning and Approach
The patient is first placed in dorsal lithotomy position with laparoscopic leg
cradles such as Allen stirrups. This allows the legs to be cushioned and allows
for access to the perineum, with flexion of the knees and hips to avoid
neuromuscular injury.18 Intermittent compression devices are also placed on
the calves at this time. As basic as it sounds, having an operating room table
with ability to achieve adequate patient Trendelenburg position is of
paramount importance (Fig. 8.2.1). Trendelenburg is often 35 degrees or
greater to allow the intestine to migrate cephalad, thereby exposing the
pelvic anatomy.
Securing the patient safely on the table is often a challenge, particularly
with obese patients. We have been placing the patient directly on an egg crate
mattress secured to the operating table as described by Klauschie and
coworkers (Fig. 8.2.2).19 This allows for the use of Trendelenburg withminimal slippage and has the advantage of working even with the morbidly
obese patient without extra straps or shoulder braces that can predispose to
neurologic and other injuries in longer procedures. One particular axiom is
that the larger the patient, the greater the Trendelenburg angle that is
required for adequate visualization. Steep Trendelenburg position is not
without consequences; however, ocular complications, alopecia, as well as
nerve injury have been reported.20 Gould et al.21 reported the use of less
Trendelenburg angle in a blinded trial which lowered the angle from 40 to 28
degrees, and found no difference in the operative times for pelvic surgery
among 16 different surgeons.
Figure 8.2.1. Placement of patient in Trendelenburg position.
Figure 8.2.2. Securing the egg crate mattress to operating table.Procedures and Techniques
Total laparoscopic hysterectomy
Step 1: Placement of uterine manipulator and bladder catheter
Before instrumentation of the patient, standard prophylactic antibiotics and DVT
prophylaxis are administered. The Caprini (ACCP) score guidelines account for the
type of surgery, obesity, previous VTE, and other complicating factors such as
malignancy to determine need and dosing.22 Antibiotic prophylaxis and VTE
prophylaxis should be based on BMI (and volume of distribution), not ideal weight.
A standard Foley catheter is placed to drain the bladder during the procedure.
One can consider the use of a dual port (three-way) catheter to allow filling and
draining of the bladder when significant lower uterine segment and bladder
adhesions are anticipated or when encountered. This allows for rapid installation of
saline to delineate the borders of the bladder and prevent incidental cystectomy.
The surgeon can use blue dye if a cystotomy is encountered to assess the water
tightness of closure.
A uterine manipulator with a pericervical cup is placed to allow for greater
movement of the uterus with fewer ports to achieve the desired angles at which to
operate. For both TLH and LSH, we use the V-Care uterine manipulator (ConMed
Endosurgery, Utica, NY) (Tech Fig. 8.2.1). Other manipulators are available and may
work equally well for these procedures. The cervix is grasped with a single-tooth
tenaculum and dilated to 21 French. The manipulator is introduced and the balloon
inflated. For the TLH, the cup of the manipulator is sewn onto the cervix to assist in
tissue removal. For the supracervical procedures, the manipulator is placed without
suturing.
Tech Figure 8.2.1. V-Care uterine manipulator.
Van den Haak and colleagues23 recently reviewed 25 articles covering 10 uterine
manipulators. Interestingly, they found that though convenient, definitive
documentation of efficacy and safety was scant. Their review did not find the
“optimal” manipulator. There has also been speculation that dilatation of the cervix
and placement of any manipulator may upstage an undiagnosed uterine
endometrial carcinoma. Iavazzo and Gkegkes24 recently reported “the assumption
that uterine manipulators can induce intra-operative dissemination of tumor cells is
suggested to be a derivative of common sense. The existence of cases with
positive peritoneal cytology after uterine manipulation cannot be determined with
certainty, and whether manipulators result in metastasis at peritoneum or disease
recurrence.” In cases where it is impossible to place a manipulator, use of a
standard infant nasal suction bulb or bulb top of an Asepto syringe in the vagina will
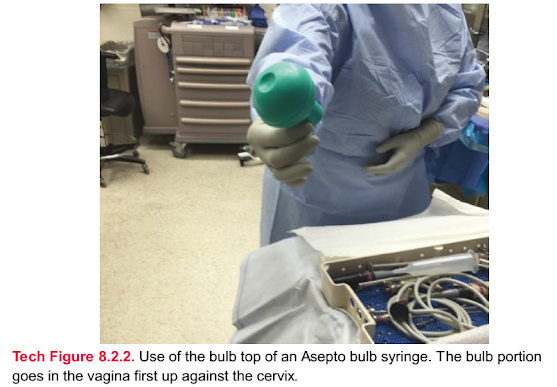
often delineate the vaginal edges (Tech Fig. 8.2.2).
Tech Figure 8.2.2. Use of the bulb top of an Asepto bulb syringe. The bulb portion
goes in the vagina first up against the cervix.
Step 2: Placement of primary trocar
Our approach to initial trocar placement is predicated on factors including uterine
size and type of previous abdominal surgery. For uteri 16 weeks pregnancy size or
less, we place the camera port at the umbilicus (Tech Fig. 8.2.3). This is a 5-mm port
for most patients, though 10-mm ports should be considered in more obese
patients to prevent damage to the instruments and camera from torque. The angle
of port insertion at the umbilicus should be 45 degrees for normal BMI patients and
more toward a 90-degree angle with increasing obesity due to the position of the
umbilicus in relation to the aortic bifurcation. We employ the direct optical insertion
technique under direct vision rather than a blind Veress needle insertion. Tinelli et
al.25 reported no statistically significant difference in complications between direct
insertion and Veress needle, suggesting that the visual entry systems offer
statistical advantage in terms of time savings and reduced minor vascular and
bowel injuries. The key concept is not to be “wed to the umbilicus” or Veress
needle.
Tech Figure 8.2.3. Standard camera port placement for uteri 16 weeks or less.
When the uterus is greater than 16 weeks size, then the camera port is placed
above the umbilicus in the midline up to a level several centimeters below the lower
costal margin (Tech Fig. 8.2.4). These should be placed at 90-degree angle to the
abdominal wall to avoid tunneling and will give greater visualization of the pelvis.
When there is a history of previous mid-abdominal or umbilical surgery such as
hernia repair with mesh or colorectal surgery, the use of Palmer’s point in the left
upper quadrant is preferable to avoid potential bowel injury on insertion.
Tech Figure 8.2.4. Port placement for larger uteri with camera above the umbilicus in
the midline.Step 3: Placement of secondary trocars
Once the patient is placed in Trendelenburg position, the abdomen is insufflated
with CO2 to a final pressure of 12 to 15 mm Hg, and the secondary ports are placed
under direct vision. If the operating surgeon is on the patient’s right side, then a 10-
mm trocar is placed in the right lower quadrant above the anterior superior iliac
spine (ASIS). The safe distances from the midline to avoid internal epigastric artery
injury are 6 cm from the midline at the level of the ASIS and 9 cm off the midline at
the level of the umbilicus.26 The exact placement depends on the size of the uterus
as this port will migrate cephalad as the uterus enlarges. The second 5-mm trocar
will be placed on the right side approximately 10 cm above the 10-mm trocar. The
third 5-mm trocar is placed on the patient’s left side at approximately the same level
as the right-sided port. If the surgeon is operating from the patient’s left side, then
the port locations are reversed. For morbidly obese patients, consideration should
be given to using all 10-mm ports to allow use of instruments with greater diameter
and avoid damage to instruments due to torque.
Step 4: Instrumentation for optimal visualization
The insufflation tubing is placed on one of the lateral ports to decrease lens
fogging. Efficient evacuation of smoke and water vapor from lysed tissue is
essential for good visualization. We employ the AirSeal (Tech Fig. 8.2.5) insufflator
(Surgiquest, Millford, CT, USA) which allows heated insufflation with CO2 and
smoke evacuation from a single port (either 5 to 10 mm). Additionally, the device is
calibrated to maintain a steady, preset pneumoperitoneum, even when the vaginal
cuff is open, which is an advantage in TLH and obese patients.
Tech Figure 8.2.5. AirSeal insufflation device.The general instrumentation used is in the standard laparoscopy sets available in
most operating rooms. Soft bowel graspers, Maryland graspers, and single- and
double-toothed tenaculums are the primary instruments for manipulation of tissue
and bowel. Electrosurgical devices are used to coagulate blood vessels and cut
tissue. We commonly use an ultrasonic device for dissection, vessel sealing, and
tissue division, as one instrument can be used for most steps (Tech Fig. 8.2.6).
Advanced bipolar devices (such as LigaSure [Covidien, Boulder, CO, USA], EnSeal
[Ethicon Endo Surgery, Somerville, NJ, USA], PlasmaKinetic, and others) can also
be used.
Tech Figure 8.2.6. Ultrasonic energy device.
Standard irrigation sets with power irrigation and suction are used to keep the
surgical field clean for dissection. In patients where there is extensive pelvic
adhesion or endometriosis, the use of lighted ureteral stents should be considered.
Placed at the beginning of the procedure, they offer a way to avoid complications
by “lighting the path” (Tech Fig. 8.2.7).
Tech Figure 8.2.7. Use of lighted ureteral stents to help with visualization of the ureters
in complex cases.
Step 5: Divide the round ligament, tube, and utero-ovarian ligament
If the ovary is to be removed, the infundibulopelvic ligament is skeletonized,
desiccated with bipolar radiofrequency device, and divided (Tech Fig. 8.2.8). The
Sonicision ultrasonic device is then used to transect the fallopian tube, round
ligament, and utero-ovarian ligament as the first step of the procedure (Tech Fig.
8.2.9).
Tech Figure 8.2.8. Inspect the pelvic structures, desiccate and divide the
infundibulopelvic ligament.
Tech Figure 8.2.9. Transect the fallopian tube, round ligament, and utero-ovarian
ligament.
Step 6: Divide the superior portion of the broad ligament
The upper portion of the broad ligament is then incised (Tech Fig. 8.2.10) and the
bladder flap is developed by opening the anterior leaf and deflecting the bladdercaudally. The insufflated CO2 will help open the leaves of the broad ligament by
filling and expanding areolar tissue and sharp dissection will expose the uterine
vessels.
Tech Figure 8.2.10. Divide superior portion of broad ligament.
Step 7: Isolate, divide, and lateralize cardinal ligaments
Once isolated, the uterine artery and veins are desiccated with bipolar
radiofrequency device and divided (Tech Fig. 8.2.11). Technically, the ultrasonic
devices should handle up to 7-mm-diameter vessels which include most uterine
arteries encountered, but our experience has been that bipolar cautery is often
needed for reliable bleeding control. The vessels are then “lateralized” in a series
of “V” motions to move the vessels laterally and over the manipulator cup (Tech Fig.
8.2.12). This also moves the ureter laterally and out of the surgical field.
The bladder flap is then further developed over the manipulator cup by sharp and
blunt dissection (Tech Fig. 8.2.13). This moves the bladder out of the way for the
colpotomy. Adhesions in this area are common and sharp dissection is used to
remove the bladder from the lower uterine segment and cervix. Injury to the bladder
is most common in this location. If it does occur, complete the dissection of the
bladder from the cervix with adequate margins prior to repairing the bladder. Use a
simple, two-layer closure with 3-0 polydioxanone (PDS-like) or polyglactin (Vicryllike) suture. Cystoscopy postprocedure is mandatory if this occurs to ensure
satisfactory watertight repair.
Tech Figure 8.2.11. Desiccate and divide the uterine artery and vein. A shows
desiccation of the uterine artery and vein with bipolar cautery. B shows division of the
uterine artery and vein using ultrasonic energy.
Tech Figure 8.2.12. Lateralize the uterine vessels over the manipulator cup with a “V”
technique. A: Artist rendition of placement of energy device to lateralize the vessels
over the manipulator cup with a “V” Technique. B: “v” technique lateralizing over the
lower uterine segment.
Tech Figure 8.2.13. Expose the vagina over the manipulator cup by deflecting the
bladder caudally.
Step 8: Repeat procedure on the contralateral side
Step 9: Colpotomy
Colpotomy proceeds along the manipulator cup from the vaginal attachments over
the manipulator cup using ultrasonic energy, or monopolar radiofrequency
instrument (Tech Figs. 8.2.14 and 8.2.15). The dissection is occurring over the V-Care
cup, Rumi-type manipulator, McCartney Tube, sponge on a sponge-stick, or other
device that is being used in the vagina to delineate the fornices. The uterus is
pulled into the vagina and the fundus can be used to occlude the vagina and
maintain pneumoperitoneum (Tech Fig. 8.2.16). Alternatively, the uterus can be
removed completely and a wet lap pad, wet lap placed in a glove, or similar device
can be used to occlude the vagina.
Tech Figure 8.2.14. Dissect the cervix over the manipulator cup.
Tech Figure 8.2.15. Remove the cervix from the vagina.
Tech Figure 8.2.16. Pull the uterus into the vagina to hold pneumoperitoneum in
smaller specimens.
Step 10: Vaginal cuff closure
Once removed from its vaginal attachments, the pedicles are inspected for
bleeding. We have been using a modified Richardson stitch at the vaginal angles,
incorporating the uterosacral ligaments as originally described for openhysterectomy by E. H. Richardson in 1929 (Tech Fig. 8.2.17).27 This involves
placement of a stitch in a figure-of-eight fashion at the vaginal angles and include
the distal portion of the uterosacral ligament, being careful not to include the vaginal
mucosa in this permanent suture material. Care must also be taken not to kink the
ureter when placing this stitch as it lies in close proximity. We generally use 0-
gauge prolene for this. The remaining portion of the vagina is approximated using
absorbable suture in interrupted or figure-of-eight fashion, using 0-gauge
polydioxanone or polyglactin (Tech Figs. 8.2.18 and 8.2.19). Alternatively, 0-gauge
barbed sutures, such as V-Lock, Quill, or Stratafix can be used for this purpose
(Tech Fig. 8.2.20). Care must be taken to get beyond the thermal damage to the cuff
in taking the closing bites of vagina. Care must also be taken not to incorporate
bladder, minimizing the possibility of postoperative fistula. The finished cuff is well
suspended as seen in Tech Figs. 8.2.21 and 8.2.22. To help with pain
management postoperatively, we have been using 5 cc of 2% lidocaine jelly
intravaginally at the end of the procedure. This can also be used postoperatively in
the form of 5 cc of Uroject (prepackaged lidocaine jelly) every 4 to 6 hours which
will help with some of the low pelvic pain that these patients often experienced
postoperatively, similar to its use for dyspareunia in breast cancer patients.28
Tech Figure 8.2.17. Modified Richardson stitch.
Tech Figure 8.2.18. Colpotomy closure using interrupted absorbable suture.
Tech Figure 8.2.19. Finished, interrupted, and suspended vaginal closure.
Tech Figure 8.2.20. Colpotomy closure using barbed suture. A securing the barbed
suture with the looped end of the suture and B 2 layer closure of the vaginal cuff using
the barbed suture.
Tech Figure 8.2.21. Prophylactic salpingectomy.
Tech Figure 8.2.22. Cystoscopy with fluorescein dye or pyridium. A shows Fluoresceindye shooting from theutereteral orifice with a distinctive yellow “highlighter”
appearance. B shows flow of Pyridium stained urine from the ureter.
Step 11: Handling of the fallopian tubes
If the ovaries are left in situ, we have been removing the fallopian tubes
prophylactically to decrease the risk of tubal or adnexal malignancy later in life as
recently reaffirmed by the National Cancer Institutes.29 This is done using the same
energy sources used for the rest of the hysterectomy, and involves dividing the
fimbriated end of the fallopian tube from the ovary and the remaining tube from its
mesentery. It is important to take all of the fimbriated ends, as that is the portion
associated with malignancy (Tech Fig. 8.2.21). It adds little time and morbidity to
the procedure and may confer benefits over our patient’s lifetimes.
Step 12: Handling of larger uterine specimens
Uterine specimens greater than 10 to 12 weeks pregnancy size will generally not fit
through the vagina without significant tearing and may be impossible to remove via
that route due to large fibroids or patient body habitus. For many specimens,
vaginal morcellation can be accomplished in the standard fashion using coring or
bivalve techniques to achieve specimen extraction. Because of concerns about
power morcellation, some practitioners are placing the uterus in a containment bag
before vaginal morcellation to theoretically decrease risk, though the efficacy of
their use vaginally has not been proven.
Alternatively, specimens can be removed through a small 4- to 5-cm mini-lap
Pfannenstiel incision, made suprapubically, or by extending the umbilical incision.
This will be described below under the section on Extracting the Uterine Corpus.
Step 13: Cystoscopy
It has been our practice to undertake cystoscopic examination in every patient after
a TLH, or complicated supracervical hysterectomy prior to leaving the operating
room. Though the literature on the value of this is not clear, we have found the
practice invaluable. A standard cystoscope setup is used with either a 30- or 70-
degree cystoscope. The bladder is usually filled with normal saline and the walls of
the bladder examined for injury or defect, specifically a through-and-through stitch
from the cuff closure or possible electrical injury. The ureters are inspected for
urine flow. Traditionally we used indigo carmine dye to aide in observing urine flow
from ureters, but this is no longer available. We have been using pyridium 200 mg,
by mouth prior to the procedure, or fluorescein dye (1 cc) at the time of the
procedure to evaluate the ureteral jets (Tech Fig. 8.2.22). Alternatively, one can fill
the bladder with 10% dextrose and observe the jets as the difference in viscosity is
readily apparent. This simple, 5-minute procedure, can, by identifying GU injuries,
decrease postoperative complications. Identification of issues at this juncture
allows for immediate repair rather than delayed recognition.In cases where cystoscopy setups are not available, the bladder can be filled
with saline from the abdominal irrigator set and the 5-mm hysteroscope placed
through the urethra for bladder evaluation. This gives the same information without
having to open a formal cystoscopy set which may be an issue in some institutions.
Laparoscopic supracervical hysterectomy
Step 1: See steps 1 to 8 of total laparoscopic hysterectomy in Procedure
and Techniques section
To accomplish the LSH, Steps 1 through 8 of the preceding section are
accomplished (see also Surgical Management). Once the uterine vasculature is
occluded, the uterus is amputated from the cervix at the level of the isthmus (Tech
Fig. 8.2.23). In the case of supracervical hysterectomy, we have been cauterizing the
endocervix from the vaginal side at the beginning of the procedure, prior to
placement of the uterine manipulator by using monopolar cautery as well as from
above with bipolar cautery after amputation. We then use a reusable Hulka
tenaculum or V-Care (ConMed EndoSurgery, Utica, NY) manipulator as described
above.
Tech Figure 8.2.23. Amputation of the uterus at the level of the isthmus with V-Care
manipulator in place. A shows removal of the lower uterine segment from the cervix
using ultrasonic energy. B shows the appearance of the cervix after uterine removal with
the top of the V-care manipulator visible.
Step 2: Amputation of the uterine cervix
The uterus is amputated from the cervix using an ultrasonic energy device at the
level of the internal os (see Tech Fig. 8.2.23). Alternatively, monopolar energy in theform of scissors, hook, or wire loop can be used for this purpose. Once this is
performed, the endocervix is cauterized from the abdominal side using a reusable
bipolar instrument to lessen the chance of cyclic bleeding (Tech Fig. 8.2.24). The
combination of cautery of the endocervix with monopolar cautery from the vaginal
side and this step of cautery with bipolar energy from the abdominal side has
dropped our cyclic bleeding rate to approximately 2% and will be discussed below.
Most remaining spotting postoperatively can be treated in the office by the use of
silver nitrate applied to the endocervix. The cervix is then closed abdominally using
a single stitch of 0-gauge absorbable suture such as polyglycan, a step that
prevents the leakage of peritoneal fluid from the open cervical os which can be
troublesome for the patient (Tech Fig. 8.2.25).
Tech Figure 8.2.24. Cautery of the endocervix with bipolar energy.
Tech Figure 8.2.25. Closure of the cervix with polyglycan suture.
Step 3: Extraction of the uterine corpus
Prior to the FDA Black Box warning on the use of power morcellators in 2014, all
specimens would have been handled by use of a power mechanical morcellator
placed through one of the port sites. We had been using the lower quadrant port
sites for this purpose to enhance visualization and make it easier to track loose
fragments. Though not currently available in many institutions due to the FDA
warning, some practitioners continue to use power morcellators by morcellating the
uterus in a specimen bag to minimize the spread of aerosolized tissue. Current
data is unclear as to whether or not this is efficacious.
What we have been doing to remove the retained supracervical specimen is
utilize some form of mini-laparotomy with a self-retaining wound retractor in the
suprapubic area with a 4- to 5-cm incision or use the umbilicus with a 2.5-cm
extension.
For the suprapubic incision (Tech Fig. 8.2.26), a 4- to 5-cm incision is made above
the pubis in the midline much as one would plan a Pfannenstiel incision. Bovie
monopolar cautery is then used to open the subcutaneous fat and open the fascia.
The peritoneal cavity is then entered with the insufflation gas still on to keep the
bowel out of the way and facilitates insertion of the retractor. A GelPort retractor is
placed through the incision (Tech Fig. 8.2.27). Once this is in place, the gas is turned
off, and the specimen is drawn into the incision and externally morcellated with a
series of “C” incisions which will elongate the specimen and allow it to be
systematically removed from the cavity (see Tech Figs. 8.2.28 and 8.2.29, Video
8.2.1). We have been able to remove specimens greater than 3,000 g in thismanner (Tech Fig. 8.2.30). It is unclear as of this writing whether the use of bag
actually adds safety to the procedure. The use of the GelPort allows for reinsufflation after specimen removal to affect a washout of the peritoneal cavity or
check pedicles. Closure of the mini-laparotomy is done in the standard fashion and
the incision can be injected with local analgesics or liposomal lidocaine (Experal)
which will impart analgesia to the incisions for approximately 72 hours, allowing for
performance in the outpatient setting (Tech Fig. 8.2.31). Alternatively, one can just
close the mini-Pfannenstiel in standard fashion and then re-insufflate.
Tech Figure 8.2.26. 4-cm mini-lap Pfannenstiel incision.
Tech Figure 8.2.27. Placement of GelPort self-retaining retractor.
Tech Figure 8.2.28.A: Bring specimen into retractor and start morcellating. B: Uterine
specimen removed by external morcellation.
Tech Figure 8.2.29. Uterine specimen being removed with a “C” technique of external
uterine morcellation. A: artist rendition of uterine specimen being removed with a “C”
technique of external morcellation and B: “C” technique to remove large specimens.
Tech Figure 8.2.30. Removal of large volume of tissue through mini-lap incision.
The umbilicus may also be a reasonable site for extraction. The umbilical incision
is made around the top or bottom of the umbilicus and extended to half way around
(or through the central portion of the umbilicus if it is large enough). The fascia is
then incised and the peritoneal cavity opened. The fascia can be extended by use
of an omega incision extending the tails out to get more space. This allows
placement of a 12-mm or 15-mm endobag to draw the uterus up to the incision and
keep it contained near the incision. Again, continuous small “C” incisions are made
in the specimen to remove it through the small incision. As with the GelPort, the
GelPOINT Mini (Applied Medical) can be used in the umbilicus (or anyplace else) to
re-insufflate and continue other parts of the procedure if necessary.
As in the section on Total Laparoscopic Hysterectomy, the fallopian tubes are
removed to lower ovarian and tubal cancer risk.
Tech Figure 8.2.31.Inject 4-cm incision with Exparel or other analgesic and close.Pearls and Pitfalls
If the uterus greater than 14 to 16 weeks size, place camera trocar above the
umbilicus or left upper quadrant.
If there are suspected adhesions, place primary camera trocar above the umbilicus
or left upper quadrant.
If the bladder is adhesed to lower uterine segment, use three-way Foley
catheter and fill the bladder with saline or methylene-blue-dyed fluid to delineate the
bladder margins.
If there is cyclic spotting/bleeding post LSH, cauterize cervix from the vaginal side
and abdominal side.
If the patient is obese, use egg crate mattress on operating table to minimize
movement and place camera above umbilicus to maximize visualization. Use of
AirSeal insufflation device to aid in visualization and maintain pneumoperitoneum.
Use lighted ureteral stents to visualize the ureters and allow for safe dissection if
there is dense low pelvic adhesion or endometriosis.
Use a bulb syringe top in the vagina or infant suction if the uterine manipulator
cannot be used to delineate the vaginal fornices.
If there is low pelvic pain postprocedure, use lidocaine jelly 2% in the vaginal
mucosa at the end of the procedure and postoperatively to help with the vaginal
pain.
If there is need for cystoscopy and equipment is not available, instill saline from
irrigator into the bladder and use 5-mm laparoscope as a cystoscope.
POSTOPERATIVE CARE
In the absence of bladder or ureteral injury, or history of previous urinary
retention with surgery, the urinary catheter is removed in the operating room
and the patient undergoes standard postoperative care. Once the patient’s
postoperative pain and nausea is controlled with PO meds, and she passes a
voiding trial, the patient is discharged from the PACU with instructions for
postoperative evaluation in 2 weeks. For patients unable to urinate, which is
an occasional issue secondary to dissection, anesthesia, or concomitant
procedures, a bladder scan is performed to confirm there is urinary retention
and that the patient is not just dry from lack of fluid. A catheter is left in for 2
days and is removed in the office after a bladder challenge to avoid
overdistention and damage. A standard hemoglobin and hematocrit are
checked prior to discharge. The patient is discharged with narcotic analgesics,
nonsteroidal analgesics, and stool softeners; and in the case of TLH, vaginal
lidocaine jelly, as previously described.A large part of successful transition from the postoperative unit to home is
predicated on management of preoperative expectations so that the patient
and her family know she is being discharged on the day of surgery and what
her limitations might be. With the patient in an outpatient setting, they are
encouraged to achieve early ambulation prior to leaving. We have also found
that the use of an abdominal binder is helpful when ambulating in the
postoperative period as this gives support to the patient’s core. Early
ambulation is key in rapid recovery and minimizing complications.
OUTCOMES
Both LSH and TLH are minimally invasive alternatives for hysterectomy. Reoperation rates are equivalent in the two procedures with no differences in
intraoperative and postoperative complications, with a trend toward lower
complications in the LSH group.30 A method-specific procedure, sometimes
necessitated after an LSH, was trachelectomy for either bleeding or
malignancy, and occurs in about 2.7% of patients, and repair of vaginal cuff
dehiscence after TLH which occurred in approximately 0.7% of patients.
Einarsson and colleagues31 did a prospective quality-of-life (QOL) evaluation
in total versus LSH patients using validated QOL questionnaires. LSH appears
to provide greater improvement in short-term QOL compared with TLH. No
significant differences were noted in postoperative pain or return to normal
daily activities. Mastering both techniques will allow for continued
conversion to minimally invasive alternatives for most gynecologic
procedures and should be in all gynecologic surgeon’s armamentarium.
COMPLICATIONS
As with any procedure, complications related to laparoscopy by itself, and
complications related to the type of surgery may occur. Bojahr et al.32
published data on 1,706 consecutive LSH patients in 2006. The mean uterine
weight was 226 g with mean operative time of 91 minutes. Fifty-two percent
had previous laparotomy. Of the 1,706 procedures, there were 14 patients
that were converted to laparotomy due to size and immobility, and one for
adhesions. There were two bladder injuries and one ureter injury in an 818-g
uterus. Overall, there was a 1.2% postoperative complication rate including
infection and bleeding. Kafy et al.33 also reported on 1,792 patients
comparing complications between abdominal, vaginal, and LH. The overall
morbidity was 6.1% with one bowel injury in the laparoscopic and abdominal
hysterectomy groups, and one ureter injury in the abdominal hysterectomy
group. Vaginal hysterectomy was associated with more urinary retention and
hematoma formation. Conversion rates were 1.7% in the laparoscopic group
and 0.4% in the vaginal hysterectomy group. Re-operation rate was 0.4% inthe abdominal group with overall morbidity being low in all groups and no
reported mortality. In a 2014 Korean study, Kim et al.34 looked at an 11-year
trend in surgical complications between abdominal hysterectomy, multi-port
LH, and single-port hysterectomy. Major complications such as bladder,
ureteral, and bowel injury were most common in multi-port hysterectomy,
with vaginal cuff dehiscence making up almost half the complications in all
groups. The total number of complications was mostly in the multi-port
hysterectomy group with the single port having the least complications.
Overall, there was a 5.3% complication rate in the abdominal group, an 8.7%
rate in the multi-port hysterectomy group, and 2.4% in the single-port group,
showing that LH is achievable with low morbidity in most groups observed.
Laparoscopic removal of large uteri represents a particular challenge,
whether total or supracervical. Alpern 35 completed a retrospective analysis of
Kaiser Permanente’s experience of 446 consecutive cases over 500 g. The
mean uterine weight was 786 g (500 to 4,500). Life-threatening complications
occurred in 0.7% of cases and required re-operation in 0.45% of cases. There
were six cystotomies, and 92.8% of the cases were discharged on
postoperative day 0 with a 1.1% re-admission rate. There was no association
between perioperative complication morbidity and patient/surgical
characteristics. Uccella, in the following year, reported on a series of 71 TLH
cases with uteri greater than 1 kg as well as a literature review.36 The median
weight was 1,120 g (1,000 to 2,860) and there was a 4.2% (three patients)
conversion rate to open surgery, two for dense adhesions, and one because of
inability to place a uterine manipulator. The median operative time was 2
hours and median blood loss was 200 mL. There were two perioperative
complications; one with vaginal bleeding 10 days postoperatively managed
conservatively and one with vaginal cuff hematoma, also managed
conservatively showing that larger uteri can indeed be handled efficiently and
safely in a minimally invasive fashion.
TLH has a unique complication in the form of vaginal cuff dehiscence
postoperatively. This can happen from several days to years after surgery and
is usually brought on by vaginal intercourse. It is a matter of debate as to
whether this is secondary to the suturing technique or use of energy to the
cuff, particularly with monopolar energy. In a 2012 Italian study, Uccella37
completed a multi-institutional analysis of 12,398 patients who underwent
hysterectomy for both benign and malignant diseases, and looked at the rate
of cuff dehiscence with the various closure types. TLH was associated with the
highest number of cuff separations 23 (0.64%) versus 6 vaginal (0.13%).
Laparoscopic suturing of the vaginal cuff had the highest separation rate at
0.86% over transvaginal suturing at 0.24%. Reducing the monopolar current
from 60 to 50 W did not alter the rates. Blikkendaal38, in a retrospective
cohort Dutch study, compared techniques of laparoscopic cuff closure; lookingat incidence of dehiscence with transvaginal interrupted, laparoscopic
interrupted, or laparoscopic running suture with conventional or bidirectional
barbed suture. Their data did not show superiority of one technique over any
other. Fuchs-Weizman and colleagues39 performed a retrospective analysis of
2,382 TLH between 2009 and 2011. She reported 23 (0.96%) cuff dehiscences
and 4 had recurrent dehiscence. The type of energy, mode of closure, and
suture material did not differ between groups. Women with more extensive
procedures were at higher risk and continuous suturing of the cuff was a
probably superior to interrupted suturing in their study.
LSH has three unique complications associated with it that are procedure
specific. The first is continued cyclic bleeding since the cervix is left in situ,
likely due to retained endometrial type tissue in the endocervical canal.
Nouri40 recently published a meta-analysis on the subject revealing that there
are varying rates of postoperative cyclic bleeding in premenopausal women,
depending on the method used to prevent bleeding. There was a 16.2% rate if
nothing was done (up to 24%). Excision of the endocervix was still associated
with high levels of bleeding (14%), and the best results came from bipolar
electrocoagulation of the endocervix which dropped the level to 2.6% on
average. All cyclic bleeding postoperatively was looked at regardless of age,
BMI, presence of endometriosis or adenomyosis, and history of previous
cesarean delivery. Similarly, we have found that monopolar cautery of the
endocervix from the vagina prior to the hysterectomy, followed by bipolar
coagulation of the endocervix after uterine amputation has decreased the rate
of cyclic postoperative bleeding at Cleveland Clinic. Much of this can be
further reduced by the use of silver nitrate in the cervical os in the office for
refractory cases with trachelectomy being necessary for very few.
Prior to 2014, power morcellation had been used to remove uterine tissue
and fibroids for LSH and larger TLH that could not be removed vaginally.
Issues associated with the power morcellators were iatrogenic spread of
endometriosis and myomatosis, as well as possible upstaging of undiagnosed
carcinoma or sarcomas of the uterus and tubes. Due to concerns about
possible spread of undiagnosed carcinoma of the endometrium or uterine
sarcoma, the FDA issued a Black Box warning on power morcellators in 2014
and we are no longer using them for tissue management. Descriptions of how
to remove larger uteri and supracervical specimens are described in detail
under Step 3 of Laparoscopic Supracervical Hysterectomy in the Procedures
and Techniques section.
































Nhận xét
Đăng nhận xét